For people living with a chronic lung disease, such as chronic obstructive pulmonary disease (COPD), emphysema, chronic bronchitis or pulmonary fibrosis, having your lungs tested is a critical part of your treatment plan.
If your doctor suspects certain lung problems or wants to monitor how effective your treatment is, he or she may order a pulmonary function test.
What is a pulmonary function test?
Simply, a pulmonary function test is a way to measure lung function. There are several types of pulmonary function tests. The most common lung function tests include spirometry, gas diffusion and lung plethysmography.
Types of common lung function tests
- Spirometry
- Lung Plethysmography
- Gas Diffusion Tests
- 6-Minute Walk Tests
- Cardiopulmonary Exercise Tests
- Pulse Oximetry
Why are pulmonary function tests done?
Your doctor may order pulmonary function tests (PFTs) to determine how your lungs are working. If you have a chronic lung disease or a condition that affects your lungs, your doctor may use pulmonary function tests to monitor your condition and treatment plan.
Pulmonary function tests can help your doctor diagnose respiratory issues such as asthma, allergies, chronic bronchitis, respiratory infections, lung fibrosis, COPD, bronchiectasis and others.
What happens during a pulmonary function test?
Your pulmonary function test may include spirometry, which measures the amount of air you breathe in and out. For some people, the procedure is outpatient, meaning you could go home the same day.
However, a pulmonary function test may be done as part of a longer hospital stay. If you have a history of lung or breathing problems, you may feel tired and will be given a chance to rest after the test. Your healthcare provider will talk with you about your test results.
A pulmonary function test can be done with two methods: spirometry and plethysmography. A spirometer is a device with a mouthpiece hooked up to a small electronic machine, and in the plethysmography, you sit or stand inside an air-tight box that looks like a short, square telephone booth to do the tests.
What does a pulmonary function test measure?
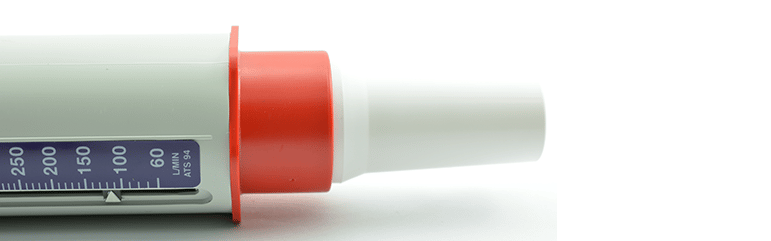
A pulmonary function test can measure lung size, air flow, lung volume, lung diffusion and more. Specifically, the pulmonary function test called spirometry measures how much air you inhale, how much air you exhale and how quickly you can exhale it.
The pulmonary function test called lung plethysmography measures the amount of air in your lungs after taking a deep breath and the amount of air that remains in your lungs after exhaling as much as you can.
Measurements Gained from a Pulmonary Function Test
- Forced Vital Capacity (FVC)—Total amount of air you can exhale after taking the deepest breath you can.
- Forced Expiratory Volume in One Second (FEV1)—Amount of air you can forcefully exhale during the first second of the FVC test.
- Total Lung Capacity (TLC)—Total amount of air in the lungs after you take a deep breath.
- Forced Expiratory Volume (FEV)—Amount of air forcefully exhaled during the first, second and third seconds of the FVC test.
- Peak Expiratory Flow Rate (PEFR)—Measures how fast you can exhale. Estimated values depend on gender, ethnicity, height, weight and age.
- Forced Expiratory Flow (FEF)—Flow or volume in the middle of an exhalation.
- Functional Residual Capacity (FRC)—Amount of air that remains in the lungs after you breathe normally.
- Maximum Voluntary Ventilation (MVV)—Amount of air you can inhale and exhale in one minute.
- Minute Volume (MV)—Amount of air exhaled per minute.
- Vital Capacity (VC)—Total volume of air you can breathe out after inhaling as much as you can.
- Tidal Volume (VT)—Amount of air inhaled or exhaled during normal breathing
What are the risks and benefits of having a pulmonary function test?
Pulmonary function tests are not invasive, and PFTs are considered safe for most people. However, all procedures have some risks.
While unlikely to occur, possible risks associated with pulmonary function tests may include:
- Dizziness
- Coughing
- Shortness of breath
In some cases, a person should not have a PFT, so it’s important to discuss any questions or concerns you have with your doctor.
Knowing and keeping track of how your lungs are doing will help you and your doctor develop or modify your treatment plan. Because lung diseases are chronic and progressive, it’s important to monitor how your treatment plan and condition are doing.
If you have a PFT that indicates your treatment plan isn’t working as well as before, you and your doctor can modify it before your condition worsens. This will keep you feeling better and staying healthier.
What can I do to prepare for a pulmonary function test?
Ask your doctor to explain the type of pulmonary function test you will have, and discuss your questions or concerns with your doctor. Your doctor may tell you not to take certain medications prior to the test. Before the test, your doctor may also advise that you:
- Stop smoking
- Not eat a heavy meal
- Wear loose fitting clothing
- Stop taking certain medications for a little while (as instructed by your doctor)
During the test, you will be given specific instructions to follow. Always follow the directions as best you can and ask questions if something is unclear.
You may be asked to repeat the test after taking a bronchodilator. You may feel tired after the test, and you will be given time to rest. After the pulmonary function test is completed, your doctor will go over the results with you during an office visit.
Taking steps to breathing easier.
In addition to monitoring your respiratory function with a pulmonary function test, taking steps to stay healthy will help your lungs. Eating a healthy diet, taking your medications, seeing your doctor regularly, getting regular exercise and trying alternative treatment.
Always consult with your doctor to find the right treatment plan for you.

Christine Kingsley, APRN is the Health and Wellness Director at the Lung Institute where she focuses on providing helpful online resources for people looking for information on various lung diseases, breathing exercises, and healthy lifestyle choices. She advocates for holistic care that involves working with your doctor to explore all options including traditional and alternative care while focusing on diet and exercise as proactive measures.









